 BBC
BBC
Excessive and severe nausea and vomiting is known as hyperemesis gravidarum and is thought to affect 1-3% of pregnancies
About 80% of pregnant women experience morning sickness, according to the NHS, with some expectant mums having such extreme nausea that they struggle with daily life. After reporter Beth Parsons was diagnosed with hyperemesis gravidarum (HG) during her pregnancy, she has been been speaking to other women affected by the condition.
Drawing the curtains to block out a warm summer's afternoon, I did everything I could to avoid being sick for the 10th time that day and wondered when I'd feel myself again.
It's isolating, lonely and very hard to describe to someone, especially when the "normal" version of morning sickness is seemingly considered a right of pregnancy passage; something that ginger, an early night and just getting past the first trimester will fix.
I've always wanted to be a mum, and my husband and I were over the moon about the positive test, but it wasn't quite the welcome to pregnancy we had in mind.
A hyperemesis gravidarum diagnosis followed.
While books and social media posts were describing the nutritious diet that would best help my growing baby, a lot of the time I couldn't even keep water down.
I would sip ice-cold cordial and suck ice lollies to keep dehydration at bay the best I could. Sometimes I would nibble on toast or dry cereal then try to go to sleep in the hope it would stay down.
 Beth Parsons/BBC
Beth Parsons/BBC
Beth Parsons experienced serious HG symptoms from week five to week 17 of her pregnancy
It was all happening at a time when internally I felt so lucky to be starting a family, and was desperate not to come across as ungrateful.
After seeing my GP, I eventually found a medication which helped and it was like a light had finally been turned back on.
For the first time in months, I was able to leave the house, return to work and started to eat and drink with more normality. I'm now in week 26 and I haven't been seriously sick since week 17 of my pregnancy.
After opening up about the issue online and in conversation, other women shared their experiences with me.
I noticed how different they were, especially when it came to what support was available and what treatments they were able to access.
In particular, the drug that helped me, commonly known as Xonvea, was often held back from women who desperately wanted to try it.
Three women shared their stories with me.

Sarah Goddard says she was being ill up to 20 times a day
Sarah Goddard, from North Yorkshire, became pregnant for the second time in August 2024.
Already mum to a four-year-old, she had been fairly sick in her first pregnancy, but HG was never mentioned. The second time round, she was seriously unwell.
"By seven weeks, I wasn't able to keep anything in me at all… I was being sick 15 or 20 times a day. I was retching to the point blood was coming out. There was nothing left in me to give.
"At times I thought I was dying, it definitely felt like that, but I thought maybe I was being dramatic, until my mum said to me, 'I think I'm watching you die'."
The 32-year-old went to hospital three times for anti-sickness injections and intravenous rehydration, but would deteriorate again as soon as she got home. She was offered some medication, but it did not work well enough for her.
"I didn't know how I was going to get through this and ultimately at 10 weeks we made the impossible decision to have a termination."
Sarah said she was "still devastated" about the decision she felt that she had to make when she chose to end her pregnancy due to the severity of HG.
"Giving my daughter a sibling was exactly what I was doing it for, and I tried and then took it away.
"I just didn't see how we were going to make it through because nobody was fighting for us. It's something I will feel guilty about until the end of time."

The NHS says about 80% of women experience morning sickness
She has now received grief counselling and mental health support through the charity Pregnancy Sickness Support.
Sarah also sought advice from a medical consultant who told her about HG and enabled access to medication so she felt able to try a third pregnancy.
She is now due to have a baby in 2026 and has thanked the consultant, saying "without him, I wouldn't be sat here, 31 weeks pregnant, with my little girl's brother".

Millie Fitzsimons was off work for eight months and lost 3st in weight
Millie Fitzsimons, 28, had HG symptoms throughout her pregnancy and experienced how different treatment options could be from one location to another.
In total she thinks she was admitted to hospital about 16 times.
She was living in Boston, Lincolnshire, when she discovered she was pregnant.
"It does just feel like you're dying… it's a feeling you can't explain. I've lost 3st in weight, was being sick 40 times a day. You're just exhausted all the time, and just sleeping on and off all day. Horrific."
 Millie Fitzsimons
Millie Fitzsimons
Millie says she ended up in hospital about 16 times
Millie said support was "really hard to get" and often medical staff would roll their eyes and not listen to her.
She tried lots of medication, including steroids which are not advised as a long-term option.
At about 16 weeks, she got help from Pregnancy Sickness Support who advised her to ask for Xonvea medication.
She said the medical staff had "never heard of it", and it took four months from asking to be able to access the medication. She could only receive one week's worth at a time.
"They just said it was a postcode lottery and it was really expensive."
When she moved to York at the end of her pregnancy in April, she was able to access Xonvea.
Her baby was born in May. She was off work for eight months while she was pregnant and does not think she will ever have another child.
The charity is campaigning for Xonvea to be included on all drug formulary to avoid issues with access.

Ella Marcham says the condition gives a "life-ruining level of sickness"
Ella Marcham from Yeadon in Leeds experienced the first symptoms of HG before she even knew she was pregnant.
Already mum to two toddlers, dealing with the debilitating condition while also taking care of her family was not easy.
"For me, the worst thing was the nausea. It never stopped," the 28-year-old said.
"It was just 24/7 - all the time. It made it really difficult for me to eat and drink properly, to parent my children, to just live my life normally… it's very difficult to describe."
 Ella Marcham
Ella Marcham
Ella struggled to care for her two toddlers while pregnant with her twins
She asked her GP and a hospital in Leeds for Xonvea, but was told they could not prescribe it. Other medication had limited success.
"The midwives tried their hardest, but we were just met with loads of barriers from doctors and it was just 'no, we can't prescribe it in this area'.
"I was at such a low point I didn't push back much because I just didn't have it in me at that point... I just sort of went a bit inside myself because I just didn't have the energy to carry on asking and asking and asking for something."
Ella briefly researched whether she could access the medication privately, but when online prices online started at £86.95 for less than one week's supply, she gave up.
She gave birth to twins in July and immediately stopped feeling sick.
Ella and husband Joe said dealing with newborn twins and two other children was significantly easier than dealing with hyperemesis gravidarum.
What is hyperemesis gravidarum?
HG patients suffer severe nausea and vomiting, which often means being sick multiple times a day, being unable to keep food or drink down, and no longer being able to continue with daily life.
The condition is thought to affect 1-3% of pregnancies, and often results in dehydration and weight loss.
Many sufferers will require medication and intravenous fluids.
If you have had HG before, it's likely you will have it in another pregnancy.
There is a variety of medications available to people experiencing HG.
Pregnancy Sickness Support has broken them down into first, second and third-line medication categories.
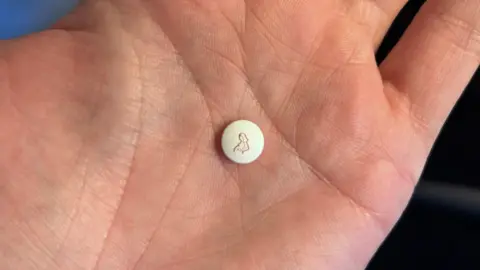
It suggests one of the first medications people should be offered is Xonvea, scientifically known as doxylamine succinate and pyridoxine hydrochloride.
It has been licensed in the UK since 2018, and is the only anti-sickness drug licensed for use in pregnancy in the UK.
 Beth Parsons/BBC
Beth Parsons/BBC
Xonvea is the only anti-sickness drug licensed for use in pregnancy in the UK
Other first-line medications include cyclizine, promethazine and prochlorperazine.
Second-line medications include metoclopramide, ondansetron and domperidone - some of which can have negative side effects for both mother and baby.
Third-line medications are usually steroids which are often successful for treating HG in people when other measures have failed.
There is a wide variety of possible side effects for both mother and baby, but the charity says it's important to remember that if HG is not treated it may cause more harm to the baby than possible effects of a medicine, including steroids.
Intravenous (IV) fluids can be used during HG to correct dehydration. Medication can also be given through an IV port if medication is unable to be kept down.
'We're extremely cautious'
Doncaster GP Dr Dean Eggitt said he sees a woman suffering from hyperemesis gravidarum "every couple of weeks".
"When women present with hyperemesis, usually we undertake an assessment of hydration. Are they drinking? Are they weeing? Are they able to go about their daily functions?
"It may be simple things like looking at what is being eaten, what is being drunk, possibly ginger biscuits, simple stuff like that. If none of that's appropriate or it doesn't really work, then we move on to medicines."
He says the first line medicine is cyclizine and Xonvea tends to be a second or third line medication.
"It has a licence to be used in pregnancy, which means that there's been research undertaken to know that it's safe to use but in medicine we doctors are slightly more cautious than that," he says.
"In a pregnant woman and an unborn child we're extremely cautious about using a medicine that's new to the market.
"So in some cases what you will find is that the local medicines management team has sat down and said, well, first of all, is this cost effective?
"Second of all, do our GPs know how to use it? And third of all, do we think that our colleagues are going to be confident to prescribe this new drug or should we let it bed in a bit first just to prove that it's safe?"
"So in theory, yes, it's safe. In reality, we can sometimes be a bit more cautious, but that cautiousness is a postcode lottery."
The Department of Health & Social Care has been contacted for a comment.
- If you have been affected by any of the issues raised in this story, information and support can be found at the BBC's Action Line.
.png)
 2 hours ago
2
2 hours ago
2








 English (US) ·
English (US) ·